In a recent study published in Allergy, a group of researchers summarized the literature on climatic hazards linked to greenhouse gas emissions and their impact on atopic dermatitis (AD).
Background
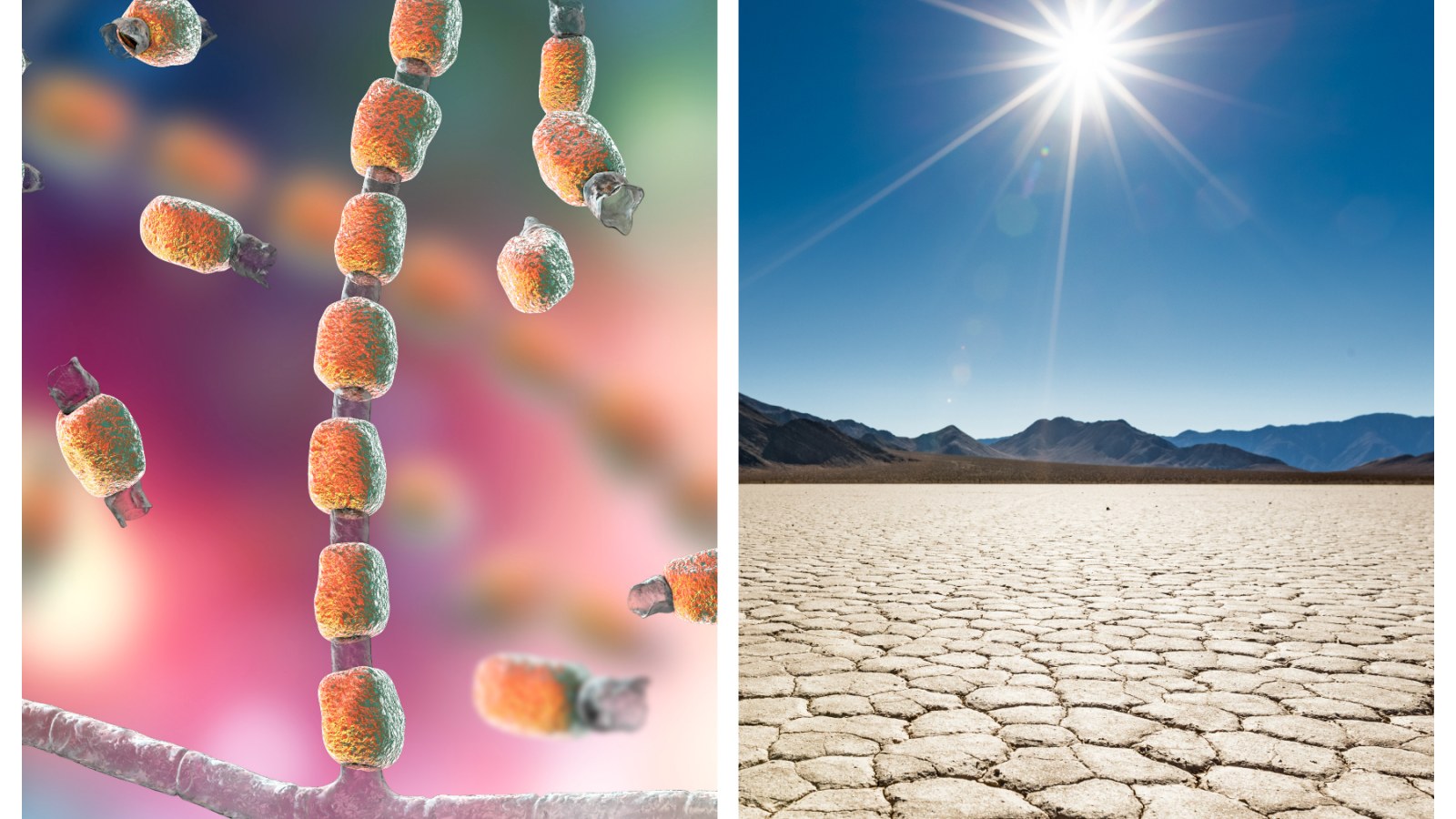
AD, a common and burdensome skin condition, is characterized by an itchy rash affecting quality of life, with onset varying from childhood to adulthood. Environmental factors like ultraviolet (UV) radiation, temperature allergens, and humidity directly impact the skin barrier, microbiome, and sensory and immune systems.
UV exposure can cause skin damage and inflammation, but at suberythemogenic levels, it offers beneficial effects against AD. Extreme temperatures trigger inflammation and skin barrier dysfunction. Toxins and pollutants disrupt the skin barrier, causing oxidative stress and inflammation.
Individuals with AD are more vulnerable to these environmental impacts due to skin barrier impairment, immune dysregulation, dysbiosis, and chronic pruritus, which are exacerbated by climatic factors.
Further research is needed because existing studies predominantly focus on single climatic hazards impacting AD without considering the complex interactions between various climatic events, and data are lacking for many world regions, especially those projected to face the most significant climatic challenges.
About the study
In the present study, the researchers employed a systematic approach to screen literature for studies examining the impact of climatic hazards linked to greenhouse gas emissions on AD.
Although they did not conduct a formal systematic review and meta-analysis due to the heterogeneity of the literature, they focused on studies that connected any aspect of AD, such as its pathogenesis, prevalence, health care utilization, incidence, and severity, to climatic hazards related to greenhouse gas emissions.
They utilized a standardized search string effective for AD research, along with search terms for ten specific climatic hazards, in databases like Embase PubMed and Google Scholar as of April 2023.
The researchers extracted information such as the study’s location, type of AD outcome measurement, focus on children versus adults, the studied and theoretical mechanisms linking climatic hazards to AD, and the outcomes’ effects on AD. The selection and summarization of the articles were collaboratively done by pairs of coauthors.
To visualize the impact of climatic hazards on AD, the researchers created maps showing the Cumulative Climate Hazard Index (CCHI) and AD prevalence. The AD prevalence data were sourced from the Global Burden of Disease study, which compiles morbidity and mortality data related to diseases. The CCHI provided a relative indication of the extent of changes in the ten specific climatic hazards in any given location globally, based on the World Climate Research Programme’s data.
They plotted the global cumulative exposure to climatic hazards in 2005 and compared it with the estimated annual percentage change in AD prevalence in the following decade. Similarly, they examined the global cumulative exposure to climatic hazards in 2017 alongside AD prevalence data from the same year and projected exposure for 2053, assuming current practices and no mitigation of greenhouse gas emissions continued.
Study results
The present study revealed a complex relationship between AD and various climatic hazards. A total of 18 studies were identified, exploring different aspects of AD, including severity, prevalence, health care utilization, and even public interest measured through Google search volume. These studies were geographically diverse, covering areas like Europe, Africa, the United States, and Asia.
The research found mixed outcomes regarding the impact of warming on AD, with some studies indicating an increase in symptoms and others suggesting a decrease. No specific studies that examined the relationship between heat waves and AD were identified. Wildfires, increasingly common due to climate change, were found to exacerbate AD, with studies showing increased rates of clinic visits and symptoms during wildfire events.
Droughts were linked to AD through indirect effects like food insecurity and psychological stress, although direct studies were lacking. The effect of precipitation on AD was found to be complex and region-specific, with some studies showing increased risk and others finding no association.
Only one study was identified that examined the impact of storms on AD, indicating an increase in outpatient visits following storm events. The relationship between floods and AD was also explored, with studies suggesting increased dermatitis visits and emergency room admissions post-flooding.
The study did not find direct evidence linking sea level rise, ocean climate change, or land cover change to AD, though these factors could theoretically impact the condition. The researchers also graphically represented the cumulative exposure to climatic hazards and its correlation with changes in AD prevalence, highlighting the potential impact of climate change on AD.
Conclusion
Overall, the findings underscore the complex interplay between climatic hazards and AD, suggesting that these relationships vary geographically and are influenced by a multitude of factors.
- Wang S-P, Stefanovic N, Orfali RL, et al. Impact of climate change on atopic dermatitis: A review by the International Eczema Council. Allergy. 2024.
doi:10.1111/all.16007 https://onlinelibrary.wiley.com/doi/10.1111/all.16007